Why sex education for providers matters.
When is the last time your doctor or nurse practitioner asked you about your sex life?
Who can you turn to when you want basic information about your sexual anatomy or functioning? Or if you have a problem?
Why is it that the average woman with pelvic pain will need to wait 8 years for a diagnosis, let alone find effective treatment?
How often are women told that they shouldn’t worry about not feeling desire for sex, “just have a glass of wine and relax”?
It’s easy to get frustrated and even apoplectic when listening to folks talk about their experiences looking for help with sexual health concerns. Maybe you have experienced this yourself.
SEXUAL HEALTH IS NOT JUST STI AND PREGNANCY PREVENTION
The problem of sexual healthcare begins with how we have historically defined sexual health. Historically sexual health has just meant avoiding infection and pregnancy.
But we all experience sexuality as far more complex and richer than just the avoidance of disease and pregnancy. Any definition of health in relation to sex must include some appreciation for the lived experience of sexuality, not just as problems to be avoided, but as a positive and universal aspect of human experience.
In the western world, health has generally been defined only in terms of the absence of disease. This is the so-called medical model. There is no doubt that this model has improved health in innumerable ways. But a definition based solely on the negative offers no guidance to the positive – to what the experience of living a healthy life would be.
Nowhere is this more obvious that when it comes to sexual health. If healthy sex lives aren’t just about risk prevention or harm reduction, how can we begin to offer a broader, more respectful, frankly sexier definition?
A more expansive definition has been offered by the World Health Organization in 2006, ““…a state of physical, emotional, mental and social well-being in relation to sexuality; it is not merely the absence of disease, dysfunction or infirmity. Sexual health requires a positive and respectful approach to sexuality and sexual relationships, as well as the possibility of having pleasurable and safe sexual experiences, free of coercion, discrimination and violence. For sexual health to be attained and maintained, the sexual rights of all persons must be respected, protected and fulfilled.”
A state of physical, emotional, mental and social well-being in relation to sexuality? That’s quite a statement from an international public health organization.
Wait, did they actually include the word ……..?!
Some 15 years later, it is still revolutionary. This is just one definition; I invite you to think about what sexual health means to you.
Definitions matter because it is only by understanding the full breadth and depth of sexuality, that all aspects of the lived experience can become relevant This expanded definition requires real change in healthcare, starting with how our healthcare team is educated.
IT BEGINS WITH SEX EDUCATION
Medical education and the training of nurses and nurse practitioners might not seem like the most revolutionary or interesting of subjects. I can’t claim that it is sexy topic.
But this training is important because ultimately it determines what “matters” in healthcare and what support you will find for your sexual health concerns at your next visit to the clinic.
It may surprise you to learn that doctors only get an average of 3-10 hours of education directly related to sexual functioning and how to have conversations about sex.
Medical education sets the stage not only for what doctors know now but also for what is deemed worthy of research and therefore how our knowledge of human health will grow into the future. Ultimately, basic education and training forms the back drop of advanced training and specialization.
Why should you worry about the effect of a new medication on female sexual response, if you don’t have a good understanding of that response to begin with?
For that matter, why should you worry about sexual physiology and orgasms when during surgery on a vulva?
What is the value of research into understanding the effect of a hysterectomy on women’s sex lives?
It all comes back to making the basics of sexuality a standard part of every provider’s education. What are the basics? That list may be long but it should at least include:
- Being comfortable discussing sex and assuming it is important to every patient until proven otherwise
- Knowing sexual anatomy and physiology, including the clitoris and pelvic floor muscles
- Understanding sexual function and dysfunction, how to diagnose it and how to treat it
GETTING COMFORTABLE TALKING ABOUT S.E.X.
Do health care providers know how to talk with patients about sex?
Certainly, they receive some training in how to take a patient history, how to break bad news, how to be “therapeutic” in conversation? It is possible your doctor or nurse practitioner even had an opportunity to practice talking about sex along the way.
But is this training adequate to meet patient’s needs?
To me, the proof is in the pudding. When is the last time a healthcare provider talked to you about your sex life and any concerns you may have about it?
Maybe you have had this experience. Maybe it even went well. But the data shows that most doctors simply are not talking about sex at all.
Primary care providers aren’t talking to their patients about sex, surveys suggest that sex is only brought up about 10-20% of the time.
Gynecologists don’t perform much better. Yes, gynecologists. The ones whose specialization is in vulvas and vaginas. Yes, those guys. Surveys show that they ask about sexual function, about problems in sex or pleasure, only 40% of the time.
What about when a woman gets breast cancer or even cancer of the vulva or vagina? I am sad to report that even then…EVEN THEN…providers are even more unlikely to talk to women about sex.
There are lots of reasons for this. Lack of training is high on the list, as is a belief that women will be uncomfortable discussing sex or that if they had a problem they will bring it up themselves.
The first step is training. But healthcare professionals also need to know that women care about sex. Talking about sex doesn’t make women squeamish – no one is going to get the vapors and faint. Women actively want their doctors to bring it up, they deserve no less.
This discussion focuses on the lack of support for women’s sexual health but ultimately sexual health conversations need to be inclusive of and affirmative for all genders, relationship styles, sexual orientations, ages, abilities, and lovers of all types of sexual play. This requires that students be given an opportunity to not only learn about sex but also to reflect on their own assumptions and biases in order to show up with compassionate and even pleasure-positive attitudes.
WHERE O’WHERE IS THE CLITORIS?
The clitoris is described as the only organ in the human body that has no other function than to provide pleasure. Maybe that’s why medical textbooks have ignored it – if pleasure doesn’t matter (least we forget this is women’s sexual pleasure) then why waste precious time on this irrelevant organ?
As someone with a clitoris or someone who loves someone with a clitoris, you may beg to differ – or more pointedly, angrily demand change. It may be frustrating to have a lover who can’t find your clitoris, but to have a doctor that doesn’t know the full extent of the clitoral anatomy is not only unhelpful when it comes to addressing problems with orgasm or pain but is also dangerous.
What is the full extent of clitoral anatomy, you may ask?
Behold the clitoris!
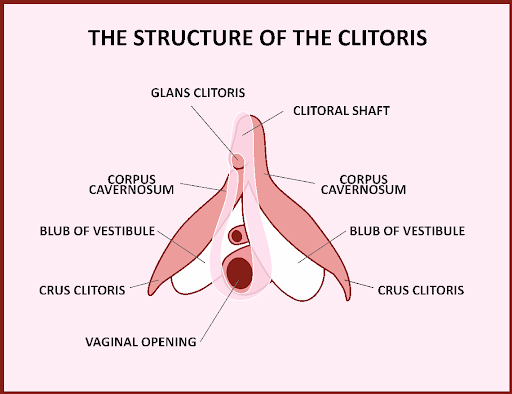
The clitoris is usually represented as a tiny wee little button of tissue towards the top of the vulva. In fact, it is a robust organ replete with two long legs and bulbs which drape around the vaginal opening. So much pleasure real estate! So much delicate tissue that can be harmed by surgeons untrained or grossly unappreciative of its sexual relevance. Just ask Jessica Pin.
Hippocrates spoke about the clitoris. Anatomists knew something about it in the 16th century and expanded on that well into the 19th century. In the twentieth century, doctors chose to forget about the clitoris. Descriptions and illustrations of the clitoris were removed but they have begun to make their way back in. Unfortunately, you may already know more about the clitoris than your doctor as they are likely to have never seen the above image. Should we blame Freud for downgrading the clitoris and saying that real orgasms only happened in the vagina? Should we get more general and just blame the patriarchy for making clitorises invisible?
It took feminist activist to re-ignite interest in the clitoris and it is taking mission-driven researchers to continue to expand our appreciation and understanding of the wonderful world of the clitoris and of female orgasm in general.
It’s not an over-statement to argue that the clitoris is a woman’s most important sexual organ (ok, maybe it’s actually the brain, but bear with me!). The fact that this is neither fully appreciated or taught in detail as part of basic education in providing health to women is indefensible.
MORE THAN KEGELS: PELVIC FLOOR MUSCLES MATTER
The pelvic floor muscles don’t fare much better that the clitoris in medical or nursing education. Pelvic floor muscles are treated like other muscles of the body – the only goal is to make them stronger. Let your muscles get weak and your urine will leak and your bladder or uterus may fall out of the vagina! Burn, baby, burn!
We have all likely heard of Dr Arnold Kegel and his exercises to prevent this catastrophe. But is this all there is to the pelvic floor?
The answer is a resounding NO! Here they are in all of their glory.
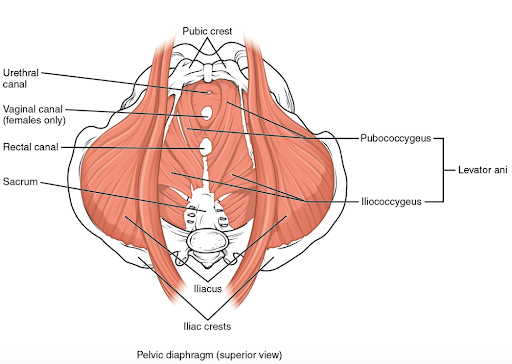
The pelvic floor muscles are a complex set of muscles that interrelate with muscles of the abdomen, hip and legs. They do indeed provide the strength and contractility needed to prevent incontinence and to help hold our pelvic organs in place.
Pelvic muscles strength is also essential to female orgasm and pleasure. Strengthening these muscles can improve orgasm intensity.
But pelvic muscles don’t just need to be strong. They also need to be flexible enough to contract and release effectively. Without these flexibility and easeful movement, pelvic floor muscles can contribute to all variety of pain in the pelvis and vulva.
The anatomy and the physiology of the pelvic floor muscles are not usually taught in any depth in medical or nursing schools, at least in terms of their relevance for female health. Importantly, simple techniques for examination of the pelvic floor muscles are also not usually explained.
Any provider who examines vulvas and vaginas should know about the complex role of the pelvic floor muscles in women’s sexual pleasure and as a major contributor to women’s pain, sexual and otherwise. If you don’t believe me, ask a pelvic floor physical therapist.
This basic information could prevent women years of unnecessary suffering from many types of pelvic pain and the devastating consequences it can have not just on women’s sex lives but on their relationships, their families, and their careers.
HOW DOES SEX WORK?
Your doctor knows something about sex. Most assuredly they know how babies are made. They likely know something about erections and how to keep penises firm.
They likely know a lot less about the most common sexual complaint from women — low desire. Low desire may seem like a minor complaint but it can cause significant distress and is a huge burden within relationships. Estimates are that approximately 10% of women feel this way, though most researchers suspect this is a gross underestimate. For midlife women, this number could approach 40%.
To understand how to support women with this problem, health care providers need to understand how desire functions. Emily Nagoski’s primer on the new science of sex is a great place to start. For example, every provider should know something about the dual control model and the differences between spontaneous and responsive desire.
This is just one concern related to one aspect of the sexual response cycle. What about women who have difficulty becoming aroused, lose the ability to have an orgasm, or have pain with sex?
How are neurotransmitters in the nucleus accumbens relevant? What about the role of the pudendal nerve? How do the parasympathetic and sympathetic nervous systems function during sex? What does embryology have to do with how women develop sexual pain?
Ultimately a deeper understanding of the basic biology of the physiological responses of desire, arousal and orgasm forms the foundation for understanding how problems arise and help direct what can be done about them.
The same mechanisms that apply to other body systems–of neurotransmitters and reflexes, of muscles and nerves, of various parts of the brain working in concert–apply to sexual function and dysfunction. Though sex is more than just about bodies in motion, understanding how bodies work in sex is fundamental to providing support towards optimal sexual health.
Of course, good sex needs more than functioning bodies. A biopsychosocial approach describes what is else is needed to understand sexuality. An approach that takes into account the BIOLOGICAL, the PSYCHOLOGICAL and the SOCIAL ASPECTS of sexual functioning.
Ultimately, providers should be trained to give the same attention to sexuality that they do to all other health concerns–to bring the same deductive reasoning, the same attention to exam and assessment, the same holistic approach, and the same commitment to finding ways to support patients right where they are.
COULD SEX ED FIX OUR HEALTHCARE SYSTEM?
Often when I meet with clients it seems that sexuality is the last space of resistance. Individuals may have anxiety, trauma, poor body image, negative thought patterns and feel disconnected from themselves and their partners. Couples may have trouble communicating, they may not appreciate each other’s needs, they may have trouble compromising or finding common ground. But somehow things keep rolling on, even if they are limping.
It is sometimes not until these issues affect sex that finally something has to be done.
Our sexual selves seem to say, “this far and no farther!” A line has been drawn in the sand. These underlying issues have to be addressed or the body will simply no longer cooperate.
Maybe one day our collective sexual selves may ultimately say the same thing to the current healthcare model.
Sure, we have limped along inadequately caring for hypertension and weight loss and diabetes within a model that jams healthcare into 15-minute appointments with over-worked and burnt-out providers.
Yes, providers have been treated like robots in a machine, dehumanized and deflated.
Yes, we have believed that the only thing that counts as “knowledge” is a statistically significant data from a meta-analysis of multiple randomized control trials.
But to come into the realm of sex, we need a different model. Sex will say, “This far and no farther!”
Sexual healthcare requires that the system has to SLOW DOWN.
Sexual healthcare requires that providers be allowed to lean into their own vulnerability and reflect on assumptions about the role of pleasure in health.
Sexual healthcare requires the system to expand their concept of “knowledge” to include data that comes from lived experience as well as rigorous scientific deduction.
slow down. Slow Down. SLOW DOWN. SLOW DOWN.
In this way, good sexual healthcare could help guide use towards how to better healthcare overall…………
These are just idle musings turned fantastical……I know. I know.
I do ultimately believe that talking about sex will change the world…even the world of healthcare!
Until this magical world emerges, I’ll be out banging my drum and educating the new generations of nurse practitioners to do better one conversation at a time.

