Let's work together to support your journey toward greater intimacy, easeful relationships, and fulfilling sex.
Your pleasure matters.
Perhaps the most common complaint of women* in my office is of pain with sex. When I am meeting with a woman around the time of menopause or after, far too often the conversations goes something like this…
Me: “Did this pain start in menopause?”
Client: “Yes, I was fine before that?”
Me: “Did your doctor or nurse practitioner ever prescribe vaginal estrogen?” Client: “Oh yeah, a long time ago but I never used it. I saw that warning about cancer in the papers that came with the prescription and it just didn’t seem like it was safe. Do you think it is ok to use?”
And almost universally, I think, “Oh no! Another woman who didn’t get what they needed for an easily treated condition because of this black box warning!”
Could vaginal estrogen really be safe?
Let’s see what the prescribing information that comes with all estrogen products says….
(https://www.nap.edu/read/25791/chapter/19#310)
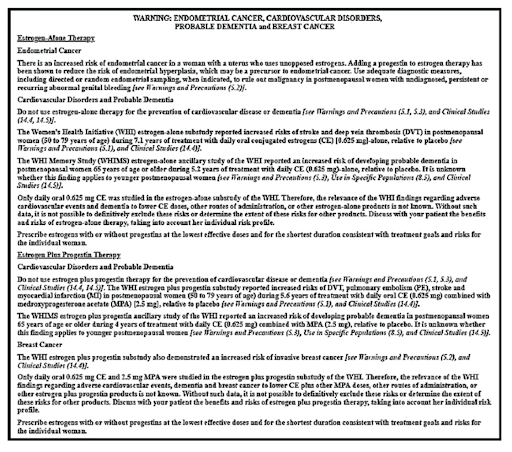
This is some fine print for sure…here is some of the text:
The Women’s Health Initiative (WHI) reported increased risks of myocardial infarction, stroke, invasive breast cancer, pulmonary emboli, and deep vein thrombosis in postmenopausal women during 5 years of treatment with conjugated equine estrogens (0.625 mg) combined with medroxyprogesterone acetate (2.5 mg) relative to placebo (see CLINICAL PHARMACOLOGY, Clinical Studies). Other doses of conjugated estrogens and medroxyprogesterone acetate and other combinations of estrogens and progestins were not studied in the WHI, and, in the absence of comparable data, these risks should be assumed to be similar. Because of these risks, estrogens with or without progestins should be prescribed at the lowest effective doses and for the shortest duration consistent with treatment goals and risks for the individual woman.
That is a pretty dramatic statement! MI, Stroke, PE, CANCER – Oh my! No wonder women are so frightened!
Since 1976 the FDA has required a package insert about the potential adverse health effects of all estrogen containing products. In fact, oral contraceptive pills were the first medication to ever have a direct to patient package insert.
The right for patients to have direct access to information about the safety of medications, rather than relying on the good will of physicians and other health care providers, was won after a hard-fought, contentious battle. You can read more about that in the excellent book The Estrogen Elixir by Elizabeth Siegel Watkins. To me, this is a straightforward positive development for patient autonomy, informed consent, and a powerful blow to the patriarcho-pharmaceutical system! Go, ladies!
But estrogens don’t just have a package insert; they have a large black box warning. A black box warning is reserved for the most dangerous of medications that have adverse reactions that may be life-threatening, fatal or disabling. Since 2003, all estrogen products have required a black box warning.
How is it that estrogen came to be thought of as a life-threatening medication?
THE WOMEN’S HEALTH INITIATIVE, ESTROGEN & THE FDA
Prior to 2001I, it was thought that estrogen had numerous health benefits and minimal risks. For example, it was believed that estrogen had minimal to no effect on breast cancer risk. It was also thought that estrogen protected women from cardiovascular disease. These beliefs were based on multiple large observational trials – but no randomized control trial (the gold standard for knowledge in the science of medicine) had been done.
Because of this high degree of safety, the numerous supposed benefits of HT, and advertising that promised that HT could keep women “forever young,” HT (in the form of Prempro) was the number one prescribed medication in America in the 1990s. I think that’s shocking! Hormone therapy was number one prescribed medication. Wow.
Enter the WHI, the first large randomized control trial to study the effect of HT on women’s health.
The Women’s Health Initiative was a landmark study in menopausal hormone therapy (HT). Over 15,000 women were recruited to study the effects of hormone therapy on cardiovascular disease, though other health effects were also monitored including breast cancer, pulmonary embolism, and gallbladder disease. The study was stopped early in 2001 due to the surprising finding that there seemed to be an increased risk of breast cancer and cardiovascular disease for women on HT.
When researchers pulled the plug on the study early and announced to the world that HT could actually increase the risk of heart attacks, strokes and breast cancer, it set off a media firestorm. It was front page news on the NY Times and the morning news. Women all over the world stopped HT. Doctors stopped discussing menopause with women, because there no longer was an effective treatment for the often-debilitating symptoms it could cause.
Of course, the FDA also noted these findings and this is how a black box warning as we know it today became mandatory on all estrogen products in the US.
SYSTEMIC HORMONE THERAPY VS LOW DOSE VAGINAL HORMONAL THERAPY
If we take it for granted that the findings from the WHI were true and indisputable (for reasons why this isn’t an easy thing to do, click here), this research only applies to the safety of systemic hormonal therapy (HT). Systemic HT refers to the use of hormones (applied directly to the skin in the form of a patch or taken orally) with the intention for the medication to enter the circulation and raise the overall body level of estrogen (and potentially progesterone).
What about using hormones just on the vagina and vulva to treat local symptoms there?
This is called low dose vaginal estrogen therapy. Unlike systemic HT, the intention is to use hormones (in the form of creams, tablets, ovules, suppositories or rings) only on the tissues of the vagina and vulva (and the urinary system, but more on that later).
Low dose vaginal hormonal therapy is therefore prescribed at much lower doses than systemic hormonal therapy – hence the name “low dose.” After all, it’s only meant to affect the area where it is applied.
For instance, the average dose of vaginal estrogen is 10mcg of estradiol (a form of bio-identical estrogen) most often used twice per week. This means that an entire year’s supply of local vaginal estrogen is equal to taking 1mg of estradiol per year. This is less than half the dose of one oral contraceptive pill. One mg of estradiol is equal to 0.01mg ethinyl estradiol found in an oral contraceptive pill.
This is low dose, real low dose. There are even versions of estradiol that go lower – down to 4 mcg.
But, medications are absorbed through the skin of the vagina, right? Even low doses of a medication could get into the systemic circulation, right?
Yes, absolutely.
But how much of the medication becomes systemic and does it matter?
As to the first question, we know that estrogen levels in the blood stream do rise transiently when local vaginal hormone therapy is applied. Research has confirmed, however, that these levels are not sustained in a range above post-menopausal levels.
Does this matter? Namely, does this transient slight increase in the level of estrogen in the systemic circulation cause life-threatening disease- as the FDA’s black box warning states in such dire terms?
IS LOW DOSE VAGINAL ESTROGEN SAFE?
Fortunately, we have excellent data available to offer a begin to offer a reliable answer to this question.
In addition to the large randomized control trial of HT described above, the WHI also had a component that was an observational trial that tracked the health outcomes for women using of systemic HT or local vaginal estrogen therapy .
This study was a doozy. Between 1992 and 2005, it enrolled 93,676 post-menopausal women. Of these, about 4,200 used vaginal estrogen alone, without systemic HT. These women were followed for on average 6-7 years.
The study found that the use of low dose vaginal estrogens did not increase the rates of cardiovascular disease, cancer or blood clots.
In 2020, researchers tallied up all of the research about low dose vaginal estrogens is compared, the finding is the same – it is effective and it is safe.
BUT WHAT ABOUT WOMEN WHO HAVE HAD BREAST CANCER?
Women who have had breast cancer often undergo treatments that seek to decrease estrogen levels in order to reduce the risk of cancer recurrence. These treatments can lead to profound vaginal dryness and discomfort.
Can women with breast cancer or with a high risk of breast cancer consider low dose vaginal hormones?
The answer to this question used to be a resounding and definitive, “NO!”
However, in recent years, the medical community has begun to reconsider this.
Several studies have suggested that there is no increased risk for breast cancer for women with or at high risk for breast cancer. The WHI Observational study found no connection. Neither did this large Finnish study. Neither did this small study from 2012.
There was enough data that in 2016, the American College of Obstetricians and Gynecologists (ACOG), stated that “The data do not show an increased recurrence among women currently undergoing treatment for breast cancer or those with a personal history of breast cancer who use vaginal estrogen to relieve urogenital symptoms.”
So, ACOG says that women with or at high risk for breast cancer can consider using low dose vaginal hormones if non-hormonal options are ineffective.
In 2020, the North American Menopause Society (NAMS) and the International Society for the Study of Women’s Sexual Health (ISSWSH) issued their updated statement. They agree that the first line treatments for GSM are non-hormonal moisturizers, lubricants and sometimes vaginal dilators. These treatments can be effective; but what if these treatments don’t work? Then the use of local vaginal estrogen can be considered.
ATTEMPTS TO CHANGE THE BLACK BOX WARNING
Based on the currently available evidence about low dose vaginal estrogens, the black box warning currently required on these products not only doesn’t protect women, but it is actually a danger to them.
Women deserve information about the safety of all medications; this is not in dispute. The problem comes when the information provided is either misleading or downright false.
False information frightens women unnecessarily and encourages them to avoid safe and effective treatments for no reason.
This is simply unacceptable.
For these reasons, the North American Menopause Society (NAMS), the international society specializing in menopause in America, submitted a petition to the FDA in 2008 requesting that the black box warning be removed from low-dose vaginal estrogen products.
Unfortunately, the FDA summarily rejected this petition, holding to their position that all estrogens are a danger despite the evidence to the contrary.
The FDA is simply misreading the meaning of the literature on the subject and refusing to heed any advice from gynecologists, menopause specialists or even oncologists. They also refuse to acknowledge the damage that their incorrect information has done to countless women’s lives.
Why has the FDA let women down in this regard? Well, it cannot be argued that the FDA has a good track record with women’s health. Whether it be with medical devices. Or excluding women from drug research trials.
I am not a willy-nilly critique of the FDA. They serve an important role in healthcare, I simply demand that they fulfill that role more effectively. Help every woman have access to safe and effective treatments for debilitating medical conditions like genitourinary syndrome of menopause (GSM).
___________________________________________________
If you are considering low dose vaginal hormones, check out this article to learn more about the type of products that are available.
But do risks associated with systemic hormonal therapy apply to low-dose vaginal creams or inserts that are used to treat GSM.
*In this article, the term “woman” or “women” will refer to people that are born with a vulva and vagina. As we know, there are women who are not born with this genitalia and other genders who do have a vulva and vagina. Language is somewhat inept in its ability to elegantly capture this beautiful complexity. I encourage you to use the information in this article as it applies to you or your loved ones.
